History
Medicine has used radiation therapy as a treatment for cancer for more than 100 years, with its earliest roots traced from the discovery of x-rays in 1895 by Wilhelm Röntgen. Emil Grubbe of Chicago was possibly the first American physician to use x-rays to treat cancer, beginning in 1896.
The field of radiation therapy began to grow in the early 1900s largely due to the groundbreaking work of Nobel Prize–winning scientist Marie Curie (1867–1934), who discovered the radioactive elements polonium and radium in 1898. This began a new era in medical treatment and research. Through the 1920s the hazards of radiation exposure were not understood, and little protection was used. Radium was believed to have wide curative powers and radiotherapy was applied to many diseases.
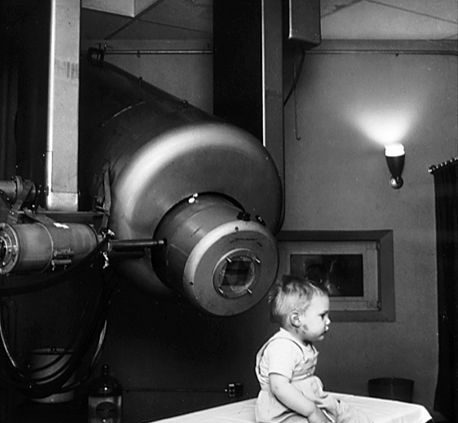
Prior to World War 2, the only practical sources of radiation for radiotherapy were radium and its “emanation”, radon gas, and the x-ray tube. External beam radiotherapy (teletherapy) began at the turn of the century with relatively low voltage (<150 kV) x-ray machines. It was found that while superficial tumors could be treated with low voltage x-rays, more penetrating, higher energy beams were required to reach tumors inside the body, requiring higher voltages. Orthovoltage X-rays, which used tube voltages of 200-500 kV, began to be used during the 1920s. To reach the most deeply buried tumors without exposing intervening skin and tissue to dangerous radiation doses required rays with energies of 1 MV or above, called “megavolt” radiation. Producing megavolt x-rays required voltages on the x-ray tube of 3 to 5 million volts, which required huge expensive installations. Megavoltage x-ray units were first built in the late 1930s but because of cost were limited to a few institutions. One of the first, installed at St. Bartholomew’s hospital, London in 1937 and used until 1960, used a 30 foot long x-ray tube and weighed 10 tons. Radium produced megavolt gamma rays, but was extremely rare and expensive due to its low occurrence in ores. In 1937 the entire world supply of radium for radiotherapy was 50 grams, valued at £800,000, or $50 million in 2005 dollars.
The invention of the nuclear reactor in the Manhattan Project during World War 2 made possible the production of artificial radioisotopes for radiotherapy. Cobalt therapy, teletherapy machines using megavolt gamma rays emitted by cobalt-60, a radioisotope produced by irradiating ordinary cobalt metal in a reactor, revolutionized the field between the 1950s and the early 1980s. Cobalt machines were relatively cheap, robust and simple to use, although due to its 5.27 year half-life the cobalt had to be replaced about every 5 years.
Medical linear particle accelerators, developed since the 1940s, began replacing x-ray and cobalt units in the 1980s and these older therapies are now declining. The first medical linear accelerator was used at the Hammersmith Hospital in London in 1953. Linear accelerators can produce higher energies, have more collimated beams, and do not produce radioactive waste with its attendant disposal problems like radioisotope therapies.
With Godfrey Hounsfield’s invention of computed tomography (CT) in 1971, three-dimensional planning became a possibility and created a shift from 2-D to 3-D radiation delivery. CT-based planning allows physicians to more accurately determine the dose distribution using axial tomographic images of the patient’s anatomy. The advent of new imaging technologies, including magnetic resonance imaging (MRI) in the 1970s and positron emission tomography (PET) in the 1980s, has moved radiation therapy from 3-D conformal to intensity-modulated radiation therapy (IMRT) and to image-guided radiation therapy (IGRT) tomotherapy. These advances allowed radiation oncologists to better see and target tumors, which have resulted in better treatment outcomes, more organ preservation and fewer side effects.
While access to radiotherapy is improving globally, more than half of patients in low and middle income countries still do not have available access to the therapy as of 2017.


دیدگاه خود را ثبت کنید
تمایل دارید در گفتگوها شرکت کنید؟در گفتگو ها شرکت کنید.